BIG PHARMA POLITICS
THE ISSUE:
EpiPen sparks consumer revolt and puts pressure on politicians to do something about rising prescription drug costs
The 500 percent jump in the price of the EpiPen focused public attention on the private struggles many consumers have faced for a while: Prescription drug costs are rising exponentially, with no end in sight.
Patients and their families who complained at the pharmacy counter or to their doctors are now collectively calling upon their elected officials for relief. In California, nurses, parents and consumer advocates campaigned hard but lost their fight for a ballot measure that would have capped prices on prescription drugs purchased by the state. In Congress, members of both parties are seeking ways to promote competition and ensure patient access to lower-cost generic drugs. In state capitols nationwide, legislators are exploring how to make drug companies more accountable by requiring greater transparency about how prices are set.
The politicians have little time to deliver. Consumers are growing impatient.
A September 2016 poll by the Henry J. Kaiser Family Foundation found 77 percent of Americans think prescription drug costs are unreasonable. There is widespread support for government to take action to keep costs down.[1]
“We need regulation of the drug industry and their pricing,” Donna Brown told Voices for Affordable Health.
Brown’s son carries the EpiPen, an emergency auto injector used to counter deadly allergic reactions. “It was always expensive,” she says. “Now the cost is sky high.”
Brown, who is retired and lives in Eugene, Ore., also worries about her own drug costs. She spends about $300 a month out-of-pocket for prescriptions.
“There has to be a better way,” she says. “It’s unreasonably cruel to profit off the disabilities of others.”
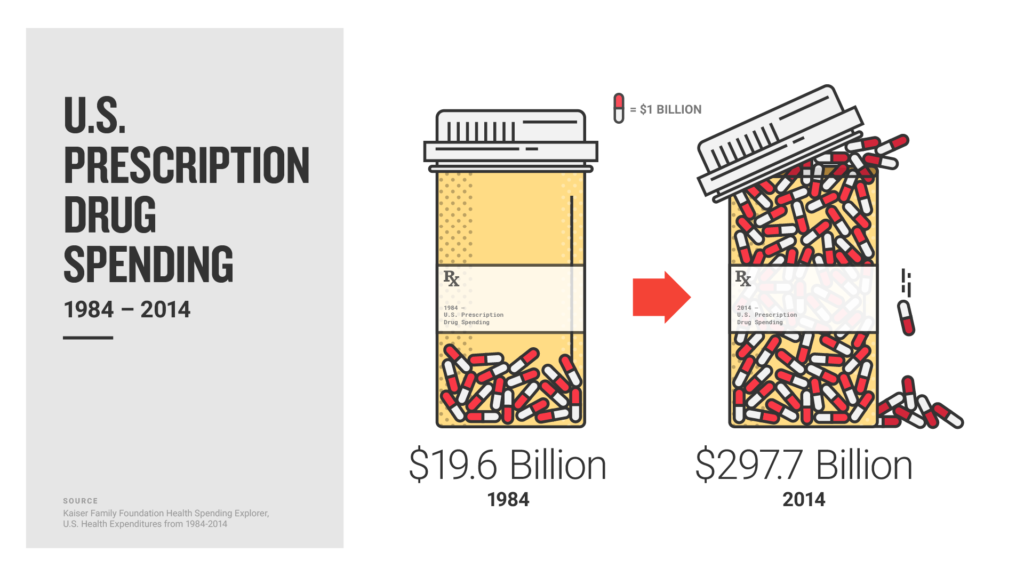
Data from the federal Centers for Medicare & Medicaid Services underscores the cumulative impact of rising prescription prices on individuals, families and taxpayers. While the number of prescription drug claims processed through Medicare grew 3.3 percent between 2013 and 2014, the costs to cover those claims increased by 17.1 percent.[2]
“Older Americans, especially those on fixed incomes, are very concerned about the rise in prescription drug prices, both brand name and generic,” says Jon Bartholomew, Government Relations Director for AARP Oregon.
“If you don’t have insurance, drug price increases can be crippling,” he adds. “If you do have insurance or are on Medicare, your share of drug costs is likely to go up, either in the form of higher percentages or higher copays. Since Medicare gets socked for the higher prices of many drugs, taxpayers also pay for rising drug costs.”
WHO IS AFFECTED:
“My insulin alone costs $2,000 a month”
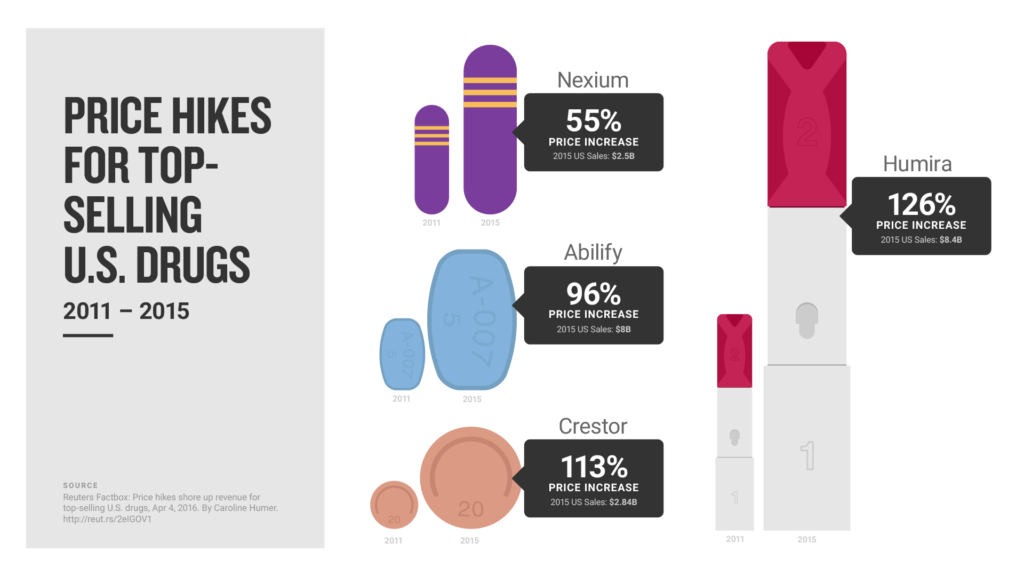
There’s no question that innovative new drugs developed by pharmaceutical companies save lives. However, there’s also growing evidence that pharmaceutical companies have steadily increased their prices, often for essentially the same product.
“Over the last several years, I have seen a price increase in my insulin every three to four months, even though this variety of insulin has now been in production for over 20 years,” Kendra Neumiller told Voices for Affordable Health.
Neumiller, who lives in Sedro Woolley, Wash., says “my insulin alone costs $2,000 a month.” After insurance, her out-of-pocket costs have grown from about $175 to $465 a month since the start of 2016.
“I have tried all of the things you hear about to reduce costs for prescriptions,” she says. “I looked at the prices at different pharmacies in my area (all within a couple of dollars of each other), contacted the manufacturer’s patient assistance program (turns out it’s only available to people without insurance), and looked at the one ‘bio-similar’ medication available.”
Her frustration is real and confirmed by hard numbers. The mean price for a milliliter of insulin increased by nearly 200 percent from 2002 to 2013, according to research published in the Journal of the American Medical Association.[3]
Dr. Tyler N. Brown of Salt Lake City, Utah, treats children who are newly diagnosed with Type 1 diabetes. In an op-ed published by the Salt Lake Tribune, Brown says the families are first hit by the diagnosis and then by the medication costs.
He notes that two large pharmaceutical companies that make insulin “are able to set their own prices, and the families whose children depend on these medications to survive must pay the ransom.”
“For the sake of those affected and for the sake of our health care system as a whole,” Brown says, “we must continue to pursue options and policies that support reasonable pricing of medications for those whose lives literally depend upon it.”
Other recent studies also document the problem:
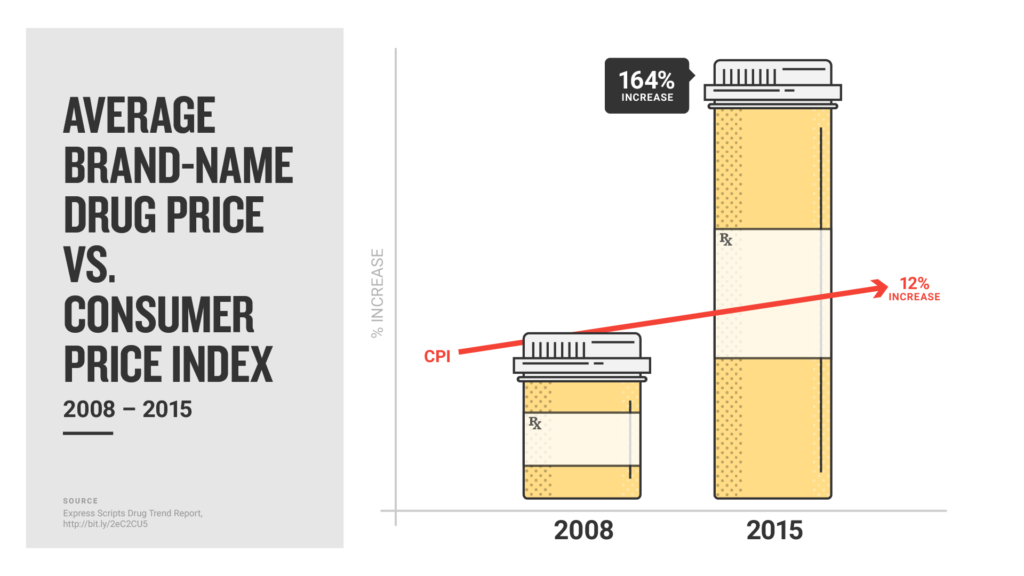
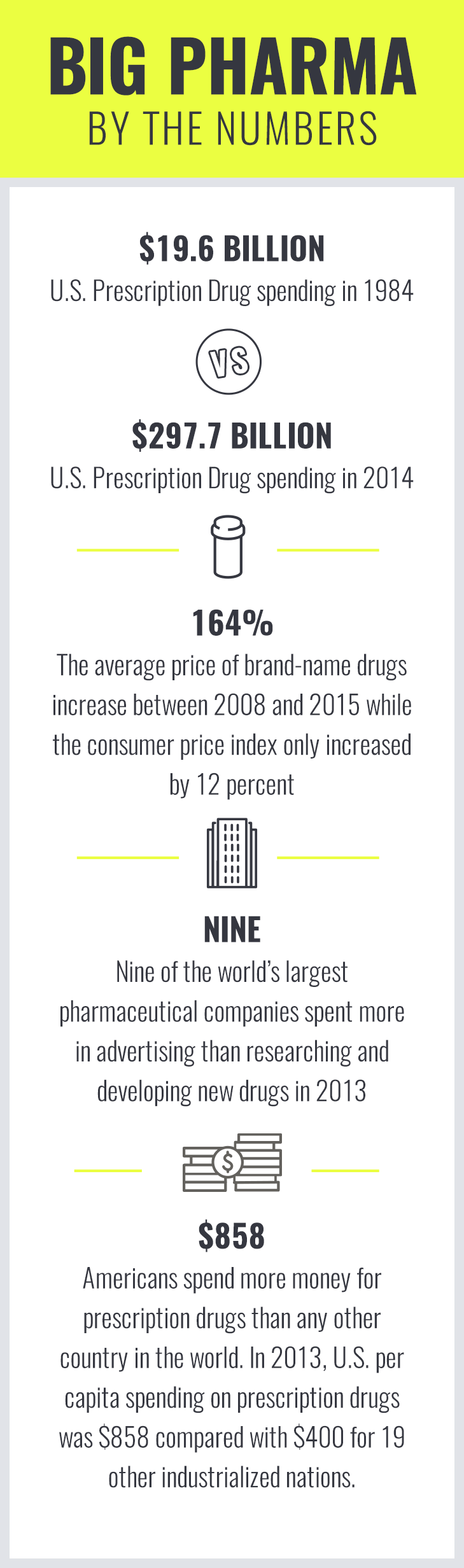
- The average price of brand-name drugs jumped 164 percent between 2008 and 2015 (while the consumer price index increased by 12 percent). [4]
- Pharmaceutical price inflation was 7.2 percent in 2015, more than twice the rate of overall medical inflation (2.7 percent) and greatly outpacing overall inflation (.7 percent).[5]
- Americans spend more money for prescription drugs than any other country in the world. In 2013, U.S. per capita spending on prescription drugs was $858 compared with $400, the average for 19 other industrialized nations.[6]
FINDING SOLUTIONS:
“We need big change and we need it now”
While the nation’s attention focused on EpiPen pricing, consumer advocates and the pharmaceutical industry battled in California over Proposition 61, the “California Drug Price Relief Act. ” The ballot measure would have required state programs such as Medicaid, the state pension program and the prison system to pay no more for prescription drugs than the U.S. Department of Veterans Affairs.
Advocates hoped it would change the rules of the game, not just in California but nationwide.
“Soaring prices for yacht club memberships don’t have much impact on the rest of us, but the pricing practices of the pharmaceutical industry can literally mean life or death,” Malinda Markowitz, a San Jose nurse and co-president of the California Nurses Association wrote in an op-ed for The Mercury News.
The California Nurses Association joined AARP and other consumer watchdog organizations in support of Proposition 61. Meanwhile, the pharmaceutical industry spent more than $100 million to defeat it. By Election Day, Proposition 61 had become one of the most expensive ballot measure campaigns in state history, with drug makers outspending proponents 8 to 1. Advocates conceded when returns showed their measure trailed 46 percent “yes” to 54 percent “no.” [7]
The pharmaceutical industry has also demonstrated its strong lobbying muscle, both in Congress and in state capitols. U.S. drug makers and their allies spent more than $880 million in lobbying expenses and political contributions to influence the nation’s response to an epidemic of drug overdoses tied to prescription painkillers, according to an investigation by The Associated Press and the Center for Public Integrity. Groups lobbying for opioid limits spent $4 million.
Drug makers also pay an army of lobbyists to defend their interests in all 50 state capitols.
Of about a dozen bills introduced in state legislatures in 2015 and 2016 that would have imposed pricing controls and transparency requirements on pharmaceutical manufacturers, just one made it into law.[8]
Still, the furor over the EpiPen and increasingly frustrated consumers may signal a turning point.
“We need big change and we need it now,” Donna Siefke of Portland, Ore., posted on Voices for Affordable Health’s Facebook page.
In September, U.S. Senators Tammy Baldwin, D-Wis., and John McCain, R-Ariz., along with Representative Jan Schakowsky, D-Ill., introduced “The Fair Drug Pricing Act.” It would require drug manufacturers to notify the U.S. Department of Health and Human Services and submit a justification report 30 days before increasing prices on prescription drugs by more than 10 percent.
In Oregon, a legislative work group spent nearly a year gathering information and debating ways to control escalating drug prices.
Draft language of a proposal to be considered by the 2017 Legislature would require drug makers to provide 90 days’ notice of any cost increase for a prescription drug exceeding 3.4 percent.
State lawmakers in Idaho, Utah, Washington and other states are also expected to renew conversations about rising drug costs. There’s growing consensus that more transparency is needed and that pharmaceutical companies should be required to disclose information related to drug development and pricing.
State legislatures will be forced to deal with budget challenges created by rising drug costs, as well as outraged constituents who have a real and personal stake in resolving the issue.
Scott DeNies , who lives in Vashon, Wash., recently shared his story with Voices for Affordable Health. His wife was diagnosed with multiple sclerosis (MS) more than 15 years ago, and today the average monthly cost for her prescriptions is $5,500.
“These drugs are all non-generic brand-name drugs, even though some have been on the market for 15 years,” DeNeis says. “U.S. law gives pharmaceutical companies the ability to patent these drugs and then charge whatever they want.”
“We need to get involved,” he says, “and urge our legislators to take this on.”
[1] Kaiser Health Tracking Poll: September 2016.
[2] Updated prescriber-level Medicare data, August 2016, Centers for Medicare & Medicaid Services.
[3] “Expenditures and Prices of Antihyperglycemic Medications in the United States: 2002-2013“; Research Letter, April 5, 2016, Journal of the American Medical Association.
[4] Express Scripts 2015 Drug Trend Report.
[5] “Trends in Hospital Inpatient Drug Costs: Issues and Challenges”, NORC at the University of Chicago, Oct. 11, 2016.
[6] “The High Cost of Prescription Drugs in the United States,” Aug. 23/30, 2016, Journal of the American Medical Association.
[7] “California Today: The Drug Industry Has Spent $109 Million to Kill Prop 61. Here’s Why.” Oct. 27, 2016, The New York Times.
[8] “States’ Efforts for Drug Price Transparency Stymied by the Pharmaceutical Industry,” The National Law Review, Aug. 2, 2016.
Did you know?…
- Consumers in the United States spend more per capita on prescription drugs than any other country
- Drug makers are now spending more than $5 billion a year on advertising—a 60 percent increase from just four years ago
- The FDA had 4,036 generic drug applications awaiting approval as of July 1, 2016, and the delay is forcing many consumers to pay high prices for brand-name drugs